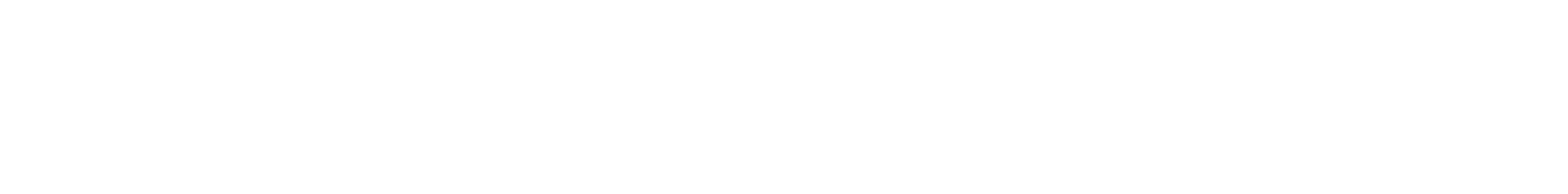
Where to begin? The model for improvement
The Model for Improvement (MFI) is a proven approach for developing, testing and implementing changes. It is used by the Institute of Healthcare Improvement as their framework to guide improvement work.
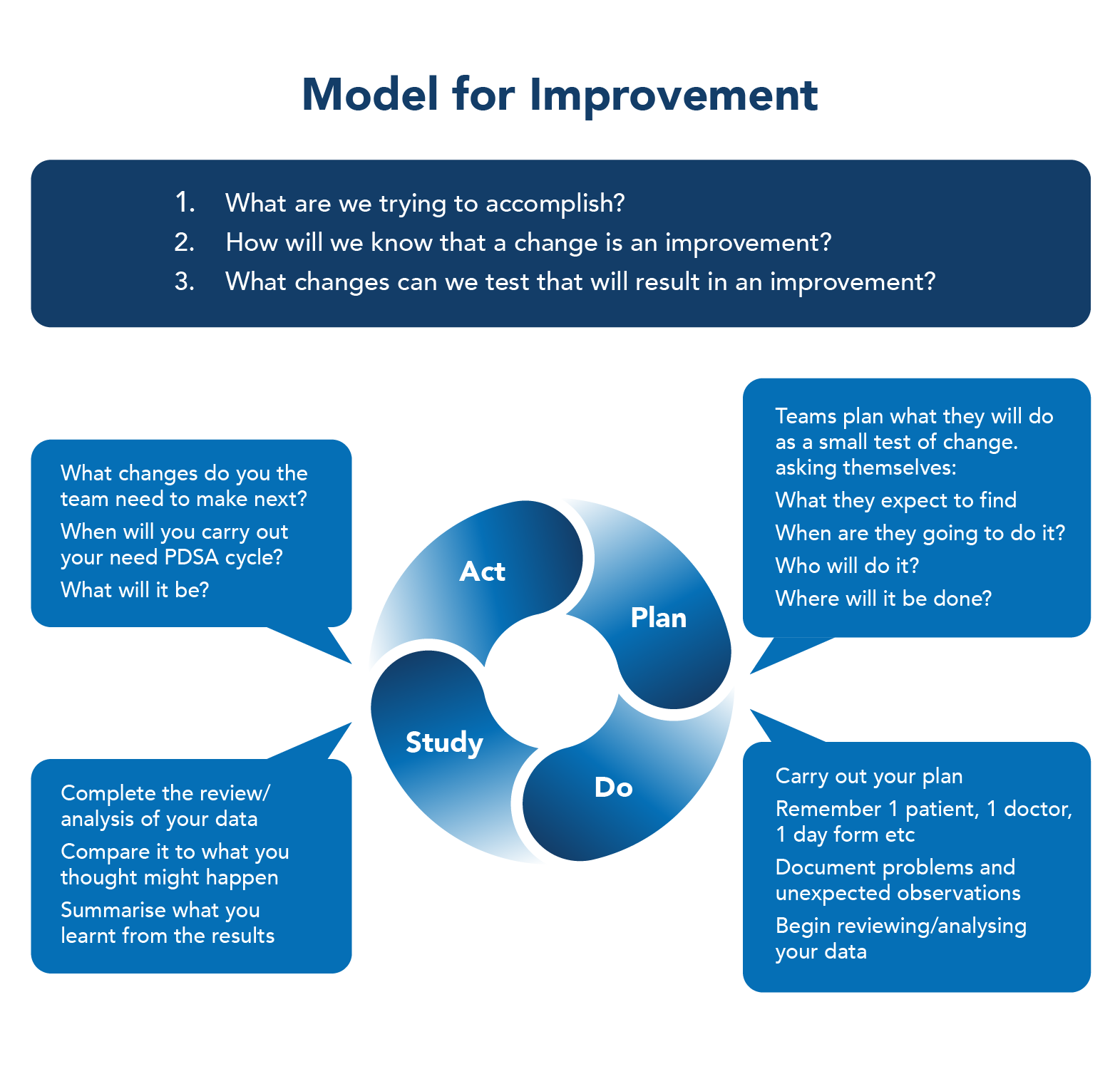
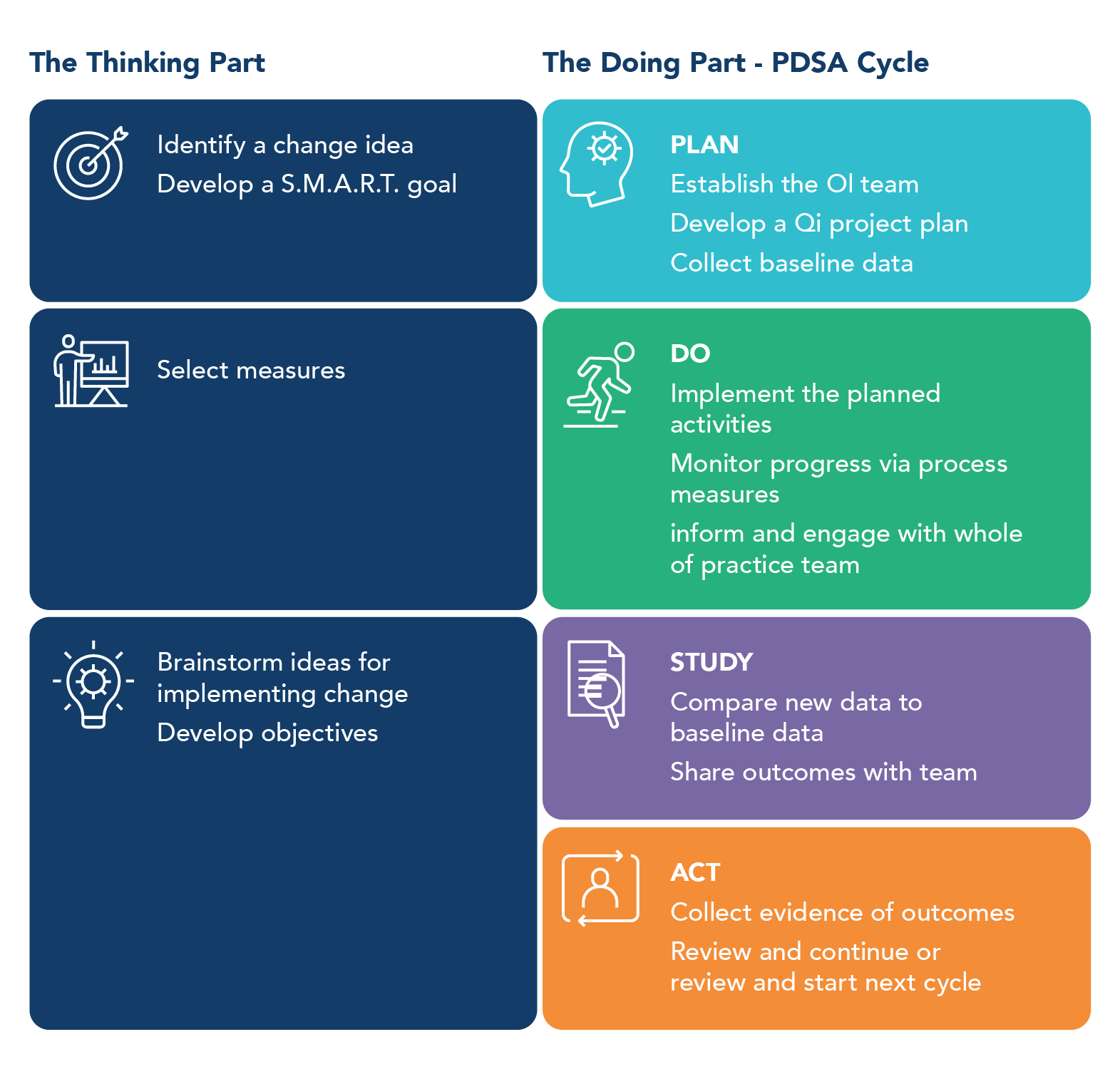
The Model for Improvement is a two-step process consisting of the thinking part and the doing part.
The thinking part asks you to answer the three fundamental questions:
- The Goal: What are we trying to accomplish?
- The Measure: How will we know that a change is an improvement?
- The Idea: What changes can we make that will result in an improvement?
The aim of these questions is to help you develop a relevant goal, and the measures and ideas that will form the basis of your activity plan.
During the doing part, you work through Plan Do Study Act (PDSA) cycles that will:
- Help you test the ideas
- Help you assess whether you are achieving your desired objectives
- Enable you to confirm which changes you want to adopt permanently
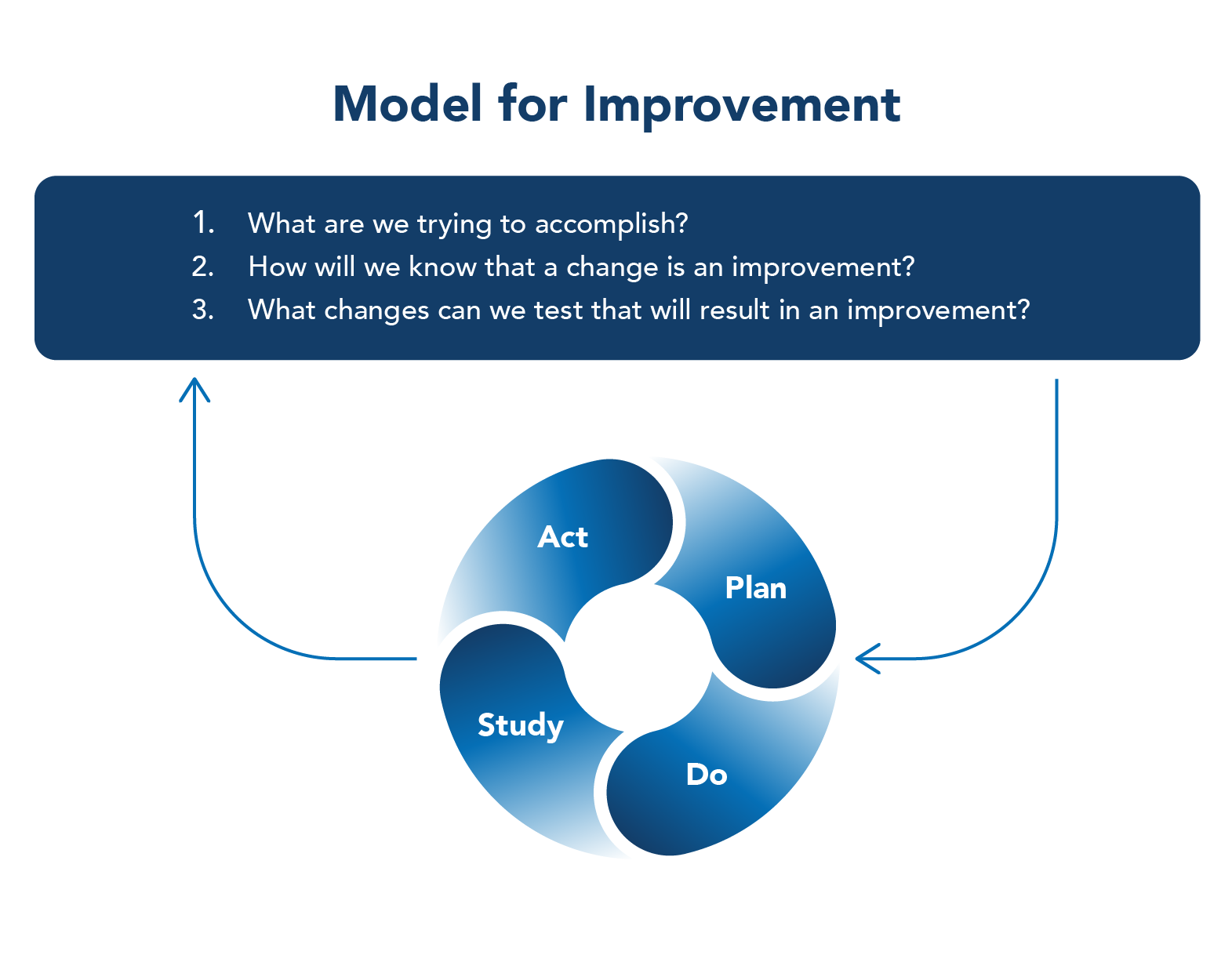
Let’s look at each step in the PDSA Cycle in a little more detail.
Step 1: Plan. In this step we define the objective and make predictions about what will happen. We develop a plan to test the change or idea by asking What? When? Who? Where? We also develop a plan for collecting data.
Step 2: Do. In this step we carry out the plan, usually on a small scale. We document observations and problems and collect the data. We also begin analysis of the data.
Step 3: Study. In this step we complete the analysis of the data and study the results. We compare the data collected to our predictions and summarise and reflect on what was learned.
Step 4: Act. In this step we refine the change, based on what was learned from the test. We determine what modifications should be made and prepare a plan for the next test. It is at this step that we also decide whether the change can be implemented without needing to run through the PDSA Cycle again.
Using PDSA Cycles enables the testing of changes on a small scale, building on the learning from these test cycles in a structured way before wholesale implementation.
This gives stakeholders the opportunity to see if the proposed change will succeed and is a powerful tool for learning from ideas that do and don’t work. This way, the process of change is safer and less disruptive for patients and staff.
Source: Model for Improvement & PDSA cycles - Clinical Excellence Commission (nsw.gov.au)